As children, many of us were told to consume calcium-rich foods like milk and cheese to grow strong and healthy bones. But did you ever consider how calcium affects your muscles?
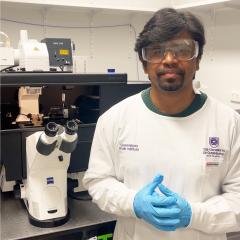
Associate Professor Bradley Launikonis of UQ’s School of Biomedical Science is on a mission to find out.
Dr Launikonis and his team are investigating the role calcium plays in regulating processes in skeletal muscle – and how it can help determine which people are likely to have adverse reactions when under anaesthesia.
“Calcium regulates processes in virtually every cell in the body and has key roles in muscle health. It plays an extremely important role in controlling the development of force,”Dr Launikonis says.
“We need to understand the basics of how calcium regulates processes in muscle, so we can find ways to promote the maintenance of healthy muscle throughout life.
“We also want to find ways to combat muscle diseases where calcium regulation is disrupted.”
While it may not be something given a lot of attention, calcium plays a huge role in how muscles fatigue, how they produce energy for continuous work and how they adapt to exercise and training.
Muscles also act as an internal heater to maintain body temperature, and this too is controlled by calcium.
As we age and our bodies change, the role calcium performs in muscle changes too.
“Muscle diseases and ageing can lead to muscle weakness, muscle mass loss, and even conditions like muscle-based hyperthermia,” Dr Launikonis says.
“This occurs as a response to external stresses – such as general anaesthetics or high environmental temperatures – in seemingly healthy people.
“These days we can obtain human muscle for our research by getting a needle biopsy from the top of the thigh, after a local anaesthetic injection. The amount of muscle taken is less than what would sit on top of the nail of your little finger.
“This technique has allowed us to study muscle from people who have mutations in a calcium channel in the muscle, which leaves them susceptible to hyperthermic reactions under general anaesthetic.
Dr Launikonis says his research team is currently working with hospitals to adapt their miniaturised biopsies to be use as diagnostics for the condition, which is genetically inherited and often requires a large muscle biopsy for diagnosis.
The adoption of these miniaturised biopsies will be a gamechanger for patients susceptible to malignant hyperthermia.
“This is important because people need to know they’re at risk, so that their anaesthetist can take the necessary precautions for their safety during a general anaesthetic,” Dr Launikonis says.
Another area of focus for Dr Launikonis is looking at how calcium influences the resting muscle and how age and exercise – or lack of exercise – influence muscle function.
“How a muscle contracts (if it is weak) can be traced back to how the muscle was ‘ready’ to contract while it was resting,” Dr Launikonis says.
“In people who have calcium channel mutations or changes in calcium regulation with advanced age, we are working with drug discovery labs in the United States to find drugs that will improve muscle function by manipulating calcium channels.”
In addition to researching resting muscle, Dr Launikonis is looking at the impact of high intensity interval training (HIIT) on muscle conditioning and function.
HIIT is known to improve cardiovascular fitness and muscle condition, but understanding just how the muscles adapt so rapidly to perform could provide insights into maintaining muscle health.
“These understandings can help people with many different conditions. Muscle is an organ that needs to function so that our whole body can be healthy,” Dr Launikonis says.
“A healthy and strong muscular system will improve a body’s capacity to combat disease and keep people independent and happy for the longest time.”